
Every diabetic person wishes to get rid of their daily medications and injections. While it may not be possible for all, a selected group of diabetic patients can achieve this with the help of surgery. Some of them can completely get rid of medications, while some may get freedom from insulin while still requiring medication. More importantly, this comes with even better blood sugar control. As with everything, here also “conditions do apply”. Read the article to understand the details and figure out what is in store for you.
A cure is a very heavy term, it may have a different meaning for each individual. To simplify, if for you cure means getting off medications and still maintaining healthy blood sugar levels, then yes it is possible. Diabetes can be cured in a selected group of patients. I would like to remind you that we are talking about type II Diabetes. Type I diabetes is a totally different disease, and we are not talking about it here.
For some who are recently detected diabetics, have an unhealthy lifestyle and are overweight, who do not have a genetic predisposition to diabetes, and whose pancreatic endocrine function is well preserved, this can be achieved simply by reducing weight and strictly following a healthy lifestyle. Someone who falls into this group should not stop treatment after reading this. Getting off medications needs to be done under the guidance of a doctor and with proper blood sugar monitoring. A lot of diabetics do this on their own, and do not check the blood sugar levels and assume that changing lifestyle will cure their diabetes. But everyone with such a profile cannot be off medications and you should not do it without the advice of your doctor.
Another group of patients who are obese and have diabetes for a couple of years can expect to be totally off medications after bariatric surgery. Again, you need to consult a bariatric surgeon for a proper assessment to know what you should expect in your case. The improvement in diabetes after bariatric surgery will depend on your age, BMI, pancreatic endocrine function, and genetic susceptibility.
Although surgery is a very good treatment option, it is not an ideal option for all. A very selected group of patients should consider this option. If you fall in the below-mentioned category then you should explore the details about a bariatric or metabolic surgery.
If you are a morbidly obese person. That is either your BMI is more than 32.5 and have diabetes with or without other obesity-related diseases. In fact, this surgery is advised to persons with BMI>37.5 even if they do not have diabetes or any other obesity-related disease.
A morbidly obese person, with BMI >32.5 and has uncontrolled diabetes even with medications should very strongly consider the option of bariatric surgery. Poor glycemic control is an indicator of ongoing damage to various internal organs of your body. It may not be apparent at present but is likely to lead to organ failures. It may be a heart attack, kidney failure, liver damage, vision loss, or foot gangrene.
To know your glycemic or diabetes control, you should keep a watch on your fasting and post-meal blood sugar levels, as well as Hb A1c levels. HbA1c level is an indicator of your average blood sugar control in the past 3 months. Ideally, it should be kept below 7 for good diabetes control. And if it is persistently >8 then it does suggest a poorly controlled diabetes.
Diabetic patients who have poor control of diabetes even with Insulin injections can consider surgery even if their BMI is in the range of 27.5-32.5. Such surgery is mainly done with the intent of achieving glycemic control and not for weight loss. And is considered as a Metabolic surgery.
The lesser the duration of diabetes, more are the chances that you can be off medications after surgery. Especially with obesity, such patients have more insulin insensitivity as the reason for their poor sugar control. The pancreatic reserve is still good. And if we intervene early, we can prevent the pancreatic burnout, which may cause irreversible damage to the pancreas.
Poor control on oral medication and the need for Insulin is an indirect indicator of the poor pancreatic beta-cell reserve. Certainly, such patients are also likely to get benefit from surgery, it is less likely that they can be a total of medications. After surgery, we may be able to achieve an Insulin free sugar control with oral medications. Or for those who have a very high insulin requirement and a poor sugar control even with insulin, surgery can reduce the insulin requirement and good sugar control.
Although it may seem that surgery is less beneficial in this group. But actually even when we are not able to get off medications totally, this is the group of patients who have the maximum benefit of surgery. As in such patients, we can prevent major organ failure, which is highly likely due to poor blood sugar control. In such patients, the risk-benefit ratio tips heavily in favor of surgery.
These are the factors that suggest the vulnerability of your pancreatic beta cells to progressive damage with time. Although these patients do benefit from surgery, these factors may be the reason for gradual decrease in the benefits of surgery with time.
Still, compared to medical therapy alone surgery has better outcomes in terms of sugar control and prevention of organ failure.
C peptide levels are the indicator of the pancreatic reserve. Many times stimulated C peptide levels are also done, to see a rise in the C peptide level after intake of sugar. Your doctor can predict the outcomes in diabetes control after surgery form these tests.
Bariatric and Metabolic surgery are technically quite similar, with some minor modifications as per the patient profile and the need. Both are laparoscopic surgeries done on the stomach and intestines. Each of them has a profound impact on the hormones and metabolism in the body.
While Bariatric surgery does lead to an improvement in diabetes, it is done on morbidly obese patients with the primary aim of reducing weight. No doubt the final goal of reducing weight is to get improvement in obesity-related diseases.
On the other hand, Metabolic surgery is done on nonobese patients, with the primary goal of improvement in diabetes. Many times technically the surgery is the same, but the term is used depending on the primary goal of surgery. While many a time minor modifications in surgery is done to get better outcomes in diabetes control and to avoid some complications.
First of all, I would like to tell the Gut that is the intestines area huge endocrine organ in itself. A large number of hormones and peptide molecules are secreted by the intestine. These hormones and molecules regulate a lot of bodily functions including blood sugar control, fat digestion, and body’s metabolism.
The blood sugar levels are affected by many hormones and metabolites apart from the insulin, that is secreted in the pancreas. Also, the production and secretion of insulin itself are regulated by other hormones and peptides produced in the intestine. Even the health and well-being of the pancreas, as well as the insulin-secreting beta cells of the pancreas, are looked after by many molecules secreted in the gut. Thus, the health of our gut, the food we eat, and the health of the bacteria in our gut have a profound impact on our overall health, including our blood sugar levels.
The changes done in the gut during bariatric surgery lead to a change in the secretion of various molecules from your gut that eventually has a positive effect on the secretion of Insulin.
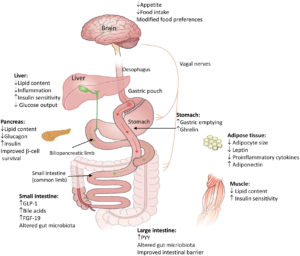
Firstly, after a bariatric surgery, food is bypassed from the duodenum, which is the initial part of the intestine adjacent to the pancreas. This change leads to an increase in the secretion of insulin and a decrease in the production of the hormone glucagon from the pancreas. The hormone glucagon works in exactly the opposite manner to insulin and hence lowering this hormone improves the blood sugar levels. Overall due to these changes, improvement in diabetes is seen immediately after this surgery.
Secondly, after this surgery, food reaches the terminal part of the intestine early. Early contact of food with the terminal part of the small intestine leads to a change in the release of some hormones and metabolites. Although this is very theoretical, for those who want to know, molecules named GLP 1 and Peptide yy are secreted in increased levels after surgery. Both of them have a positive impact on the production and release of insulin from the pancreas. Not only that they also improve the survival and growth of new beta cells in the pancreas. The beta cells are the one that produces insulin. In patients with type II diabetes, these beta cells die down early and are reduced in number.
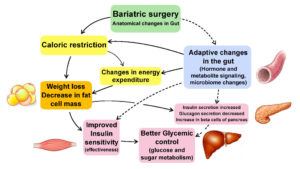
In type II diabetes, the problem is not just the reduced production of insulin. Even the insulin that is secreted is not as effective. More Insulin is used by the liver cells and muscles to absorb sugar from the blood. And this ineffectiveness is called reduced insulin sensitivity. This reduced insulin sensitivity is part of the metabolic syndrome that is seen in obese patients. In very simple words, weight gain reduces insulin sensitivity and weight loss improves insulin sensitivity or effectiveness.
Hence, after bariatric surgery, as weight is lost, gradually insulin sensitivity improves. With the improvement in insulin effectiveness, there is better control of blood sugar levels.
There is an even more important aspect of this. Due to an increase in the effectiveness of insulin, less insulin is needed to control blood sugar. And hence there is less burden on the pancreas to produce insulin. This improves the longevity of the beta cells in the pancreas. This is very important for the long-term health of the pancreas and long-term outcomes of diabetes.
Soon after surgery, even before any significant weight loss, the blood sugar levels start improving. This is due to improving insulin levels and a decrease in caloric intake. Gradually with weight loss, insulin sensitivity improves leading to further improvement in diabetes. Over a period of time, increasing beta-cell levels improves pancreatic health and gives a lasting improvement in diabetes and sugar metabolism.
Actually, improved glycemic control is just a marker that we follow and measure. Bariatric surgery also leads to similar massive improvements in lipid (fat) and liver metabolism and other hormonal systems of the body. This is seen over a period of time in good lipid profile, reducing levels of cholesterol, improving the fatty liver, and regularization of the reproductive hormone system both in males and females. Due to weight loss improvement in joint problems, stress urinary incontinence, and breathing problems are also seen after bariatric surgery.
The overall impact of this surgery is a reset in the body’s metabolic and hormonal system. In morbidly obese patients these systems have been disturbed for a long time due to an unhealthy lifestyle. And thus set into a fixed unhealthy state, leading to multiple health problems. Returning back to a healthy metabolism and hormonal balance improves the root causes of the multiple health problems faced by these patients. And so we see the magical health benefits in all the obesity-related diseases after bariatric surgery.
You need to understand that no treatment is totally risk-free, neither is wait and watch policy for any medical condition. You always have to assess the benefits against the risk and then make a decision.
Bariatric surgery is major abdominal surgery and has its own risk and complications just like any other surgery. But when done with proper evaluation, following all proper guidelines, and by an expert surgeon, these surgeries have a very low complication and mortality rate compared to other major surgeries. As it is done laparoscopically the recovery is very fast. Return to normal life is also quite quick.
Regarding the longevity of the benefit, the majority of the patients have a long-term resolution of diabetes. You need to understand that, an unhealthy lifestyle is a primary reason for obesity and diabetes. Hence, they can lead to weight regain and derangement of glucose metabolism even after surgery. So if a patient modulates his lifestyle post-surgery and adheres to the advised follow-up, he need not worry too much about long-term results. In most cases, the problems restart due to the resumption of an unhealthy lifestyle.
You should, first of all, understand the pros and cons of the surgery. Also, need to understand if you fall in their category to whom surgery is recommended, and what are the expected benefits and risks. Regarding benefits you should try to understand not just reducing medications and injections, but also the long-term benefits in avoiding organ failure due to better control of diabetes. You should ask yourself these primary questions
If you are obese and diabetic, you should certainly consider surgery. As it is highly likely to improve your diabetes. And if you have other obesity-related diseases then the recommendation for surgery is even stronger. Reduction in weight and improvement in other obesity-related diseases will be an added advantage.
If your diabetes is poorly controlled and you have got the advice for starting at insulin and you are obese, then it is time to consider surgery. Surgery not only controls sugar and avoids insulin need, but it also preserves your pancreatic endocrine function. Even if you not ready for surgery yet, you should not neglect your doctor’s advice to start insulin injections. This is the stage where if you avoid surgery and insulin both out of fear, there will be burnout of the pancreas. This will worsen your diabetic control over time.
In this case, surgery may not be able to get you off medications or even insulin. But good control of blood sugar levels will be crucial in preventing catastrophe. I feel this is the group of patients that are having the maximum benefit of surgery. Even if they need treatment for diabetes after surgery.
If you are a candidate who could benefit, you should better meet a bariatric and metabolic surgeon and discuss all your concerns. You should understand what are the possible outcomes in your case. What are the shorter and long-term benefits, and what are the risks for you. You should then be able to take a more informed decision for yourself.